Dense Breasts? Better Screening Options Exist
I have dense breast tissue.
If you've ever received a notification letter from your mammography center telling you the same thing, you probably know the feeling: confusion, concern, and wondering what you're supposed to do with that information.
When I got my notification a few years ago, the letter essentially said I had dense tissue and that it might make cancer harder to detect. But it didn't give me clear next steps or alternatives. I realized so many women are receiving these letters without understanding what they really mean for their health and screening options.
Today, I want to give you the information I wish I had received back then.
You'll learn what dense breast tissue actually means, why mammograms may not be enough, and discover five safe, effective screening alternatives backed by research. Most importantly, you'll know how to advocate for screening that actually works for your body.
In fact, this topic is so important that the FDA now requires mammography centers to notify you if you have dense breast tissue. And it's incredibly common: sixty-six percent of premenopausal women and twenty-five percent of postmenopausal women have dense breasts. You're not alone in this.
Let's dive in.
What Is Dense Breast Tissue and Why Does It Matter?
Understanding Dense Breast Tissue
Dense breast tissue simply means you have more fibrous and glandular tissue than fatty tissue in your breasts. While this is a normal variation in breast composition, it creates a significant challenge for mammography.
Here's why: on a mammogram, both dense breast tissue and tumors appear white. It's kind of like trying to find a snowball in a snowstorm. When radiologists are looking at your mammogram, they're searching for white masses (potential tumors) against a white background (your dense tissue). This makes detection incredibly difficult.
If you're wondering how common this is, you might be surprised. Research published in Radiology shows that sixty-six percent of premenopausal women and twenty-five percent of postmenopausal women have dense breasts. That means the majority of women in their childbearing years and a significant number of women after menopause are affected by this screening challenge.
The FDA Notification Requirement
The FDA now requires mammography centers to notify you if you have dense breast tissue. This requirement exists because dense tissue significantly impacts mammogram effectiveness and increases your cancer risk.
When you receive that notification letter, it's not meant to alarm you. It's meant to inform you so you can have meaningful conversations with your healthcare provider about whether additional or alternative screening methods might be appropriate for you.
Understanding that you have dense breast tissue actually empowers you to make better decisions about your screening options.
The Problem: Mammograms Miss Up to 50% of Cancers in Dense Breasts
Reduced Detection Effectiveness
The short answer to whether mammograms can miss cancers in dense breast tissue is yes.
Research published in Radiology demonstrates that mammographic sensitivity drops significantly as breast density increases. For women with the densest breasts, sensitivity can drop to just forty-eight percent. That means mammograms are missing more than half of cancers in the densest breast tissue.
Let that sink in for a moment. The test we've been told is the gold standard for breast cancer screening is only catching about half of cancers in women with very dense breasts.
The impact of this limitation has been substantial. Over a thirty-year period, the widespread use of mammography led to over-diagnosing approximately 1.3 million women in the United States. These women received treatments for breast cancers that may not have ever spread or caused harm.
Increased Radiation Exposure
Detection challenges aren't the only concern with mammography for women with dense breasts. Dense breast tissue also absorbs more radiation than fatty tissue. Some women with large or dense breasts may absorb more radiation with some women receiving more than seven times the average radiation dose.
Research published in the British Journal of Radiology raises an additional concern about mammography radiation. The low-energy X-rays used in mammograms may be four to six times more damaging to breast tissue than other types of X-rays. This suggests the cancer risk from mammogram radiation might be higher than previously understood.
The National Cancer Institute acknowledges that theoretically, annual mammograms in women aged 40 to 80 years may cause up to one breast cancer per 1,000 women.
What Leading Experts Say
I'm not alone in questioning the effectiveness of mammography, especially for women with dense breasts. Some of the most respected voices in medicine have raised these same concerns.
Dr. Otis Brawley, the former Chief Medical and Scientific Officer of the American Cancer Society, has stated that mammography is a suboptimal test and that we need a better test.
Dr. Archie Bleyer, lead author of a study published in The New England Journal of Medicine, concluded that screening is having, at best, only a small effect on the rate of death from breast cancer.
Writing in The Lancet, Dr. Peter Gotzsche stated that screening for breast cancer with mammography is unjustified.
These aren't fringe voices. These are respected researchers and physicians who have spent decades studying breast cancer screening and are calling for better alternatives.
There's even a powerful documentary called bOObs: The War on Women's Breasts that investigates this controversy in depth. The film features women sharing their experiences of how mammography failed them, along with medical experts scientifically examining the claims about early detection and low radiation that have been promoted for years.
I'm not sharing this to scare you or to tell you to stop getting mammograms. I'm sharing this because you deserve to know the full picture so you can make an educated decision about your screening options.
And the good news is, there are alternatives that can give you information about what's happening in your body, sometimes years before a tumor even forms.
5 Safe, Effective Screening Alternatives for Dense Breasts
So let's talk about what those alternatives are. These options offer different approaches to breast screening that can be more effective for women with dense breast tissue.
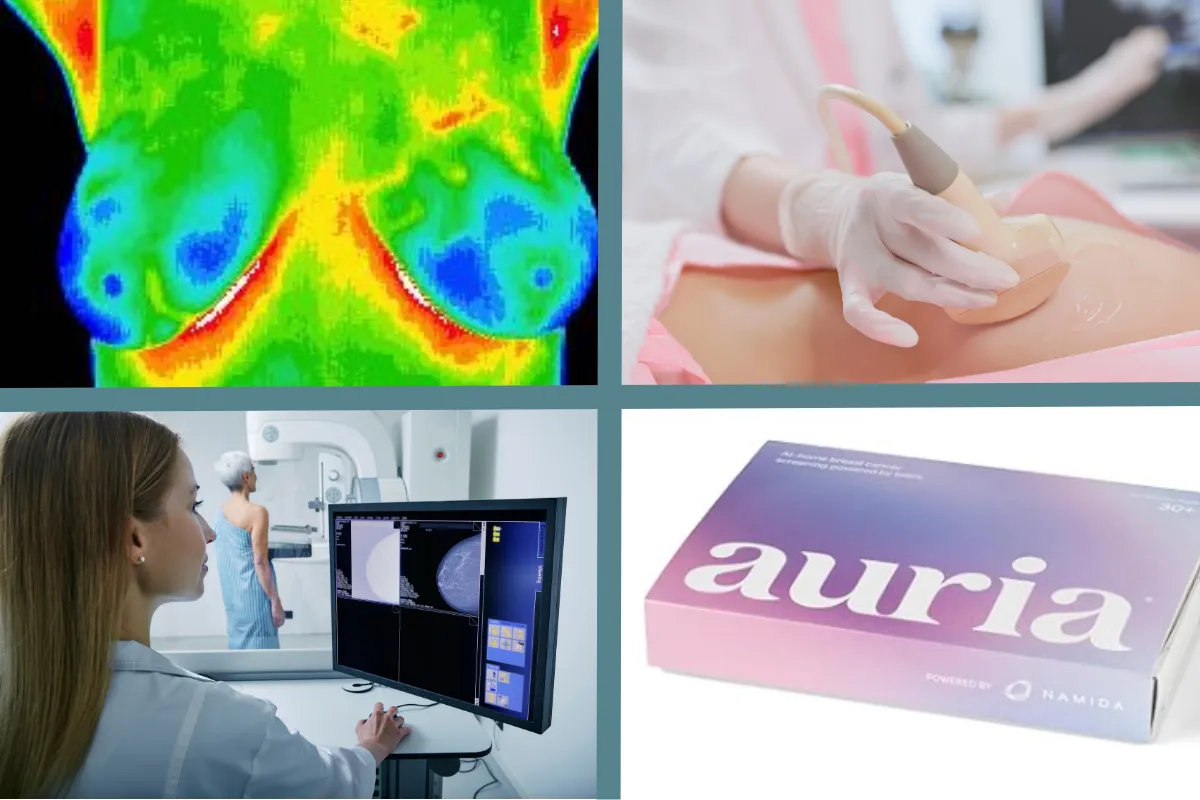
Breast Thermography (Traditional and Advanced)
Breast thermography is a screening method that takes a completely different approach from mammography. Instead of looking for tumors that have already formed, thermography looks at what's happening physiologically in your breast tissue before tumors develop.
Traditional breast thermography uses infrared imaging to detect temperature differences in breast tissue. It identifies areas of increased heat that could signal inflammation or increased metabolic activity.
Thermography has been extensively researched. A 2015 review published in PMC (PubMed Central) documented that over 800 peer-reviewed studies have been published on breast thermography, with 110+ review articles examining its clinical applications. A 2024 systematic review and meta-analysis published in PMC identified 22 qualifying studies and found pooled sensitivity of 88.5% and specificity of 71.8% for thermography in breast cancer detection.
The National Cancer Institute notes that tumors can cause temperature changes that may show up on thermograms.
Advanced breast thermography builds on that foundation with several important enhancements:
Advanced thermography uses highly sensitive digital infrared cameras that can measure minute temperature differences in your breast tissue. It uses black and white imaging to show vascularization (blood vessel patterns) in greater detail.
The images are analyzed with sophisticated computer software that can recognize patterns the human eye might miss. This advanced analysis allows for detection of subtle physiological changes and patterns that were previously undetectable.
Advanced thermography also includes Hormonal Grades, which assess estrogen stimulation in the breast tissue. This gives you additional information about hormonal activity that could affect breast health.
Advanced thermography (AI-driven or 3D infrared thermography) has a sensitivity of 88–96% and specificity between 71–90% across independent studies.
Sensitivity means the thermographic test correctly detects most cancers and rarely misses them (low false negatives). In screening, this is important to ensure no cases of early cancer go undetected
Specificity measures how effectively thermography identifies people who do not have breast cancer.
Both traditional and advanced thermography are completely non-invasive and radiation-free, making them safe options for repeated screening.
Automated Whole Breast Ultrasound (AWBUS)
Automated Whole Breast Ultrasound, commonly called AWBUS, is a computer-guided robotic system that uses a large transducer to scan your entire breast and create three-dimensional images. Think of it as a movie of your breast tissue rather than just snapshots.
AWBUS is particularly effective for women with dense breasts. Research published in Radiology shows that adding screening ultrasound can find forty percent more cancers in women with dense breasts than mammograms alone. That's a significant improvement in detection.
It provides standardized, reproducible, whole-breast coverage, which means you get consistent imaging every time. This consistency makes it easier to track changes over time and compare results from one screening to the next.
Diagnostic Ultrasound
You might also have heard of diagnostic ultrasound, which is different from AWBUS. Diagnostic ultrasound is when a technologist manually moves a smaller probe over specific areas of your breast.
It's typically used to evaluate something specific or suspicious that was found on another test. Diagnostic ultrasound provides high-definition, two-dimensional images of targeted areas and can even evaluate blood flow within lesions. This detailed evaluation makes it valuable for investigating areas of concern.
Auria Tear Test
The Auria tear test represents an entirely different approach to breast cancer screening. This is a tear-based screening method that analyzes your tears for biomarkers related to breast cancer risk.
It's non-invasive and provides another layer of information about your breast health through a simple tear sample.
QT Breast Imaging
QT Breast Imaging is another alternative screening technology that uses three-dimensional ultrasound breast imaging. The images are evaluated using artificial intelligence, which helps identify patterns and potential concerns.
Like thermography, QT imaging is non-invasive and radiation-free, offering women another option that doesn't involve X-ray exposure.
An Important Note About FDA Regulation and Insurance Coverage
It's important to note that some of these alternative screening methods are not yet FDA-regulated or covered by insurance.
But that doesn't mean they aren't valuable or effective. It often just means the system hasn't caught up yet. Many effective medical approaches and technologies take years to gain FDA approval and insurance coverage, even when backed by substantial research.
If you're interested in exploring these alternatives, you may need to pay out of pocket and advocate strongly with your healthcare provider. But for many women, having access to screening that actually works for their body type is worth the investment.
How to Advocate for Yourself with Your Healthcare Provider
Now that you know about these alternatives, you might be wondering how to actually have these conversations with your healthcare provider. Let me give you some practical steps.
First, come prepared with questions. You might ask things like, "Given that I have dense breast tissue, what are my options beyond mammography?" or "Have you heard of advanced thermography or whole breast ultrasound? Would those be appropriate for me?"
Remember, you're not being difficult or questioning their expertise. You're being a good steward of your health. Asking informed questions is part of responsible self-care.
Second, if your current provider isn't open to discussing alternatives or dismisses your concerns, it's okay to seek out providers who are more aligned with integrative approaches and who respect your desire to be informed. You deserve a healthcare partner who listens to your concerns and works with you to find the best screening approach for your body.
Third, remember this: you are the steward of the body God gave you. It's not only okay to ask questions and seek answers, it's important.
Caring for your body isn't selfish. It's responsible stewardship. You were created on purpose for a purpose, and advocating for your health allows you to fulfill that purpose with strength and vitality.
You have options. You have a voice. And you deserve screening methods that actually work for your body.
The Connection Between Breast Health and Overall Wellness
Now, breast health doesn't exist in isolation. It's connected to your overall wellness, including things like detoxification, nutrition, stress management, sleep, and movement.
When we support our body's natural detoxification processes, we help reduce the toxic burden that can contribute to inflammation and hormonal imbalances. These are the kinds of lifestyle factors that impact not just breast health, but your overall vitality and well-being.
This is where taking a holistic approach to your health becomes so valuable. Instead of just focusing on one screening method or one area of concern, you can look at the bigger picture of what your body needs to thrive.
The Wheel of Wellness and Weight Loss is a free assessment that helps you identify which lifestyle factors may be impacting your health across six key areas: mindset, sleep, stress, nutrition, movement, and detoxification.
It takes just a few minutes to complete, and it gives you a personalized roadmap for where to focus first. Instead of feeling overwhelmed by everything you think you should be doing, you'll have clarity on what your body actually needs most right now.
Frequently Asked Questions
Q: What does dense breast tissue mean?
Dense breast tissue means you have more fibrous and glandular tissue than fatty tissue in your breasts. This is a normal variation in breast composition. However, on a mammogram, both dense tissue and tumors appear white, which makes it harder to detect cancer. It's like trying to find a snowball in a snowstorm.
Q: How common is dense breast tissue?
Dense breast tissue is very common. Research shows that sixty-six percent of premenopausal women and twenty-five percent of postmenopausal women have dense breasts. If you've been notified that you have dense breast tissue, you're far from alone.
Q: Can mammograms detect cancer in dense breasts?
Mammograms can detect some cancers in dense breasts, but their effectiveness drops significantly as breast density increases. For women with the densest breasts, mammographic sensitivity can drop to just forty-eight percent, meaning mammograms may miss more than half of cancers in the densest breast tissue.
Q: What are the best screening alternatives for dense breasts?
There are several effective alternatives including advanced breast thermography (which can detect changes years before tumors form), Automated Whole Breast Ultrasound or AWBUS (which finds forty percent more cancers in dense breasts than mammograms), diagnostic ultrasound, the Auria tear test, and QT breast imaging. Each has different strengths, and many women benefit from using multiple screening methods together.
Q: Are thermography and ultrasound covered by insurance?
Many alternative screening methods, including thermography and some forms of ultrasound screening, are not yet FDA-regulated or covered by insurance. This can be frustrating, but it doesn't mean these methods aren't valuable or effective. You may need to pay out of pocket and advocate with your healthcare provider about which screening methods are most appropriate for your individual situation.
Summary: Key Takeaways
If you have dense breast tissue, here's what you need to remember:
Dense breast tissue is common. Sixty-six percent of premenopausal women and twenty-five percent of postmenopausal women have dense breasts. You're not alone.
Mammograms have limitations for dense breasts. Sensitivity can drop to forty-eight percent for the densest breasts, and dense tissue absorbs more radiation than fatty tissue.
You have options beyond mammography. Safe, effective alternatives like advanced thermography, ultrasound, QT breast imaging, and other screening methods can provide better information about your breast health.
You deserve to be heard. Come prepared with questions for your healthcare provider, and don't be afraid to seek out practitioners who respect your desire to make informed decisions about your screening.
Breast health is connected to overall wellness. Supporting your body through nutrition, detoxification, stress management, sleep, and movement impacts not just breast health but your total well-being.
You have options. You have a voice. Advocating for your health isn't just okay, it's an important part of stewarding the body God gave you so you can fulfill your purpose with strength and vitality.
Ready to Take Action?
Ready to take the next step in your wellness journey?
Download the free Wheel of Wellness and Weight Loss at inspiredwell.org/wheel. This simple assessment takes just a few minutes and will show you exactly which areas of your health need attention first. You'll get a personalized roadmap for where to focus across six key wellness areas: mindset, sleep, stress, nutrition, movement, and detoxification.
Want to dive deeper into this topic?
Watch the full video where I walk through all of this information in detail: Dense Breast Tissue: What Every Woman With Dense Breasts Needs to Know (YouTube link)
For more information and research, I highly recommend:
Documentary: bOObs: The War on Women's Breasts
Book: The Smart Woman's Guide to Breast Cancer by Dr. Jen Simmons
Interview: Dr. Jen Simmons with Jill Carnahan on YouTube
Prairie Health and Wellness Podcast: https://youtu.be/pxkCUvKTzwg?si=uID5EzH8yX5WpqxY
Looking for community support?
Join Every Woman Well, a faith-centered online space where women encourage each other and share their wellness journeys without the noise and distraction of social media. Visit portal.inspiredwell.org
Remember, you were created on purpose for a purpose. Advocate for your health, ask the hard questions, and choose what's best for your body.
Stay inspired.
References
[1] Kolb, T. M. (Lead Author). Radiology. Mammographic sensitivity for breast cancer declines significantly with increasing breast density (48% for the densest breasts). Two-thirds (66%) of premenopausal women and 25% of postmenopausal women have breasts dense enough that a mammogram will miss their breast cancer. Addition of screening ultrasound significantly increases detection of small cancers; screening breast ultrasound will find 40% more cancers in women with dense breasts than mammograms will.
[2] Heyes, G. J., et al. British Journal of Radiology. Low energy X-rays (as used in mammography) are approximately 4-6 times more effective in causing mutational damage than higher energy X-rays.
[3] National Cancer Institute. Theoretically, annual mammograms in women aged 40-80 years may cause up to one breast cancer per 1,000 women. Tumors can cause temperature changes that may show up on the thermogram.
[4] Bleyer, A. (Lead Author). The New England Journal of Medicine. Screening is having, at best, only a small effect on the rate of death from breast cancer.
[5] Gotzsche, P. C. (Lead Author). The Lancet. Screening for breast cancer with mammography is unjustified.
[6] Review article (2015). PMC. Retrieved from https://pmc.ncbi.nlm.nih.gov/articles/PMC4791361/. Documents over 800 peer-reviewed studies published on breast thermography with 110+ review articles.
[7] Systematic review and meta-analysis (2024). PMC. Retrieved from https://pmc.ncbi.nlm.nih.gov/articles/PMC11603657/. Identified 22 qualifying studies on breast thermography with pooled sensitivity of 88.5% and specificity of 71.8%.
[8] Review article (2022). PMC. Retrieved from https://pmc.ncbi.nlm.nih.gov/articles/PMC9731505/. Summarizes thermography as a significant screening modality.
[9] Miller, A. B., et al. The British Medical Journal. The data suggest that the value of mammography screening should be reassessed (specific mortality for women aged 40-59).
[10] van Netten, J. P., et al. Lancet (Letter to Editor). Compression during mammography can rupture cysts, and dissemination of cancer cells as a result of compression might occur.
[11] Hsieh, C. C., et al. European Journal of Cancer. Premenopausal women who do not wear bras had half the risk of breast cancer compared with bra users.
Additional Resources:
Smith, M. S. (Director). bOObs: The War on Women's Breasts [Documentary]. WayMark Productions.
Simmons, J. The Smart Woman's Guide to Breast Cancer.
Prairie Health and Wellness Podcast. https://youtu.be/pxkCUvKTzwg?si=uID5EzH8yX5WpqxY

